Breast cancer rehabilitation: post mastectomy physical therapy and more
26 July 2021
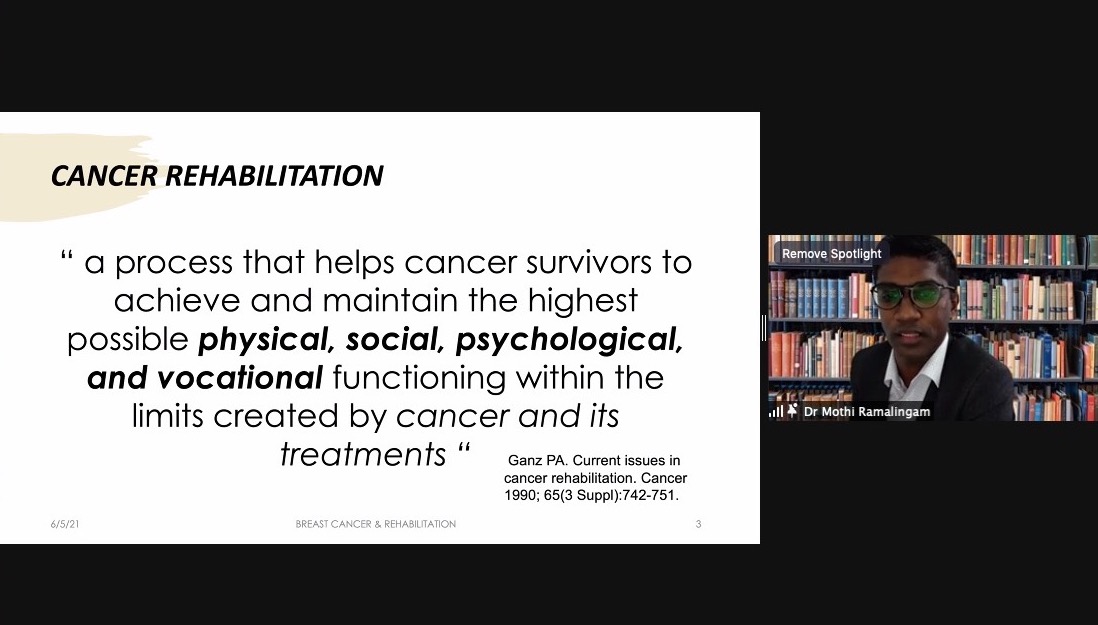
What is cancer rehabilitation?
Rehabilitation is a relatively new concept in breast cancer care that encompasses a wide range of therapies designed to maximise a person’s physical and emotional functioning with cancer. At its core, it aims to help people cope with the long-term side effects of treatment, which range from fatigue and pain to mobility issues.
Why is breast cancer rehabilitation so important?
With breast cancer survival rates on the rise - according to the Singapore Cancer Registry report released in 2017, stage one breast cancer patients have a five-year survival rate of 90 per cent, while stage two patients have a five-year survival rate of 80 per cent - there is an increasing number of patients who may experience late effects related to treatment. Such patients can thus benefit from cancer rehabilitation, regardless of their cancer stage.
“We are seeing breast cancer patients at various stages of the disease, who have the opportunity to live many good years, just like any other individual. At the same time, there are concerns about their quality of life and symptoms, which they may have to live with for the next few decades of their lives, depending on their condition. Rehabilitation addresses those issues,”said Dr Huren Sivaraj, a medical oncologist and CEO of Oncoshot.
More options for breast cancer survivors
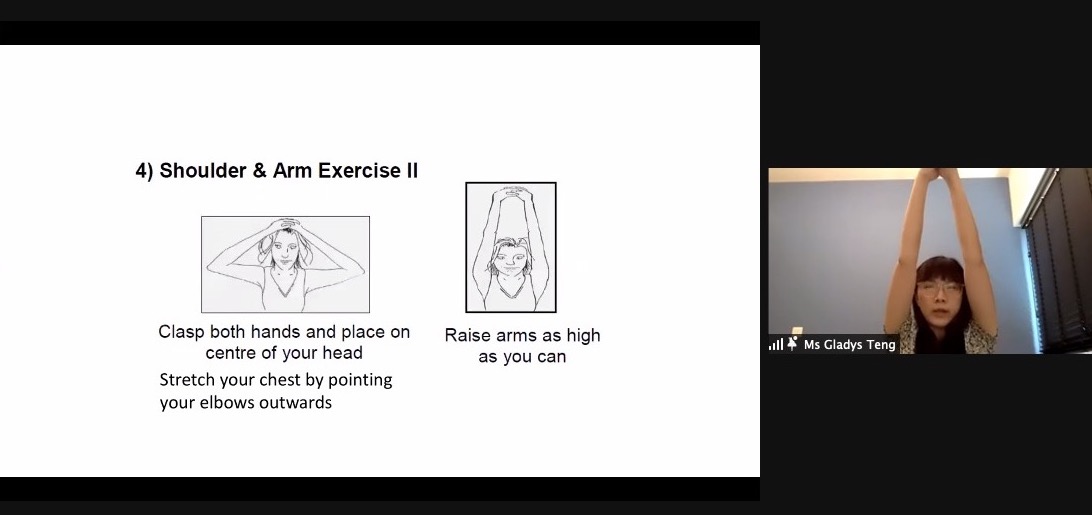
To spread awareness of breast cancer rehabilitation, Oncoshot and the Breast Cancer Foundation (BCF) recently held a webinar, which featured tips on boosting the breast cancer recovery journey from a panel of experts. This included Dr Mothi Babu Ramalingam, a consultant from Singapore General Hospital’s Rehabilitation Medicine department; Dr Tan Si Ying, an associate consultant from Singapore General Hospital’s Breast Surgery Department; Ms Gladys Teng, a principal occupational therapist from Singapore General Hospital and Ms Jamie Teo, the head of advocacy and communications from BCF.
Among the topics covered were managing post-surgery symptoms such as lymphedema, as well as exercises for breast cancer survivors. Notably, the webinar highlighted that with the lengthening of breast cancer patients’ lifespan, the field of rehabilitation - which is grounded in helping patients to improve their quality of life through options such as exercise - is set to grow in importance.
“In the future, breast cancer patients may consult a rehabilitation professional before seeing an oncologist, to find out how they need to change their lifestyle and habits, especially with regard to nutrition and physical activity. We are moving towards a new model of care, where we have rehabilitation centres within cancer centres, which we are trying to incorporate on a national level. Tele-consultations and virtual consultations will be the new norm for incorporating home-based exercise programmes, though this is still being developed,” he shared.
If you missed the webinar, here are the questions answered during the session by our panel of experts.
Why am I experiencing side effects such as numbness around the breast and inner armpit years after breast cancer surgery?
DR TAN: There are many factors that could cause such numbness, but this usually depends on what sort of surgery was done. The skin around your breast may be numb because after taking out portions of it, the nerves that pass through the breast to the skin may have been interrupted during surgery. This may cause slight numbness and a tingling sensation around the wound area, which is more sensitive, but this usually decreases over time. There is, however, a small percentage of patients who still experience this discomfort over an extended period of time.
Numbness around the inside of the armpit usually occurs after surgery is performed in the area - this involves either sentinel lymph node biopsy or axillary clearance. Sometimes, lymph nodes are stuck to sensory nerves that provide sensation to the inside of your armpit. These nerves are removed during surgery, which may cause permanent numbness on the inside of your arm. Of course, the person who knows best is the surgeon, with whom you should check on whether the numbness may be permanent.
What is your advice regarding health supplements? Is there any evidence that supports intermittent fasting during rehabilitation?
DR MOTHI: Intermittent fasting is something that is currently being studied in animal models. It focuses on reducing obesity, as there are links between glucose and cancer. However, intermittent fasting for breast cancer rehabilitation has not been explored in human trials, though it has been found to help with muscle health and reduce obesity.
We generally don’t recommend over-the-counter supplements, but most patients are placed on immuno nutrition during the prehabilitative phase, or before they start treatment. This typically includes omega, fatty acids and similar substances. We mostly try to focus on moving patients to a diet that's higher in protein, provided they don’t have symptoms that prevent them from doing so, as this can confer them with better muscle health. This means that they won’t experience worse outcomes even if the cancer progresses.
What exercises can we do during the prehabilitative phase to help with the recovery journey during neoadjuvant treatment (where patients receive systemic therapy before surgical removal of the tumour)?
MS TENG: We encourage patients to do basic exercises such as brisk walking or stretching to prevent any kind of muscle stiffness. Flexibility exercises such as yoga are also helpful. Patients undergoing treatment may feel unwell at times, so we do encourage them to start slow with low impact activities such as walking, but if they feel they can take on a little bit more, they can further discuss this with their therapist or doctors. They may be able to jog or do pilloxing exercises.
What are your thoughts on the use of Traditional Chinese Medicine (TCM) during rehabilitation?
DR MOTHI: TCM has multiple components, including the herb-based one, but non-medication-based TCM is what we have utilised to a greater extent - including acupuncture and electroacupuncture. In Singapore, we have board services in the hospital - depending on which u visit - and also medical doctors who hold TCM board certification in medical acupuncture. The latter is mainly administered for pain-related impairments or symptoms. We have also conducted a clinical trial to see whether acupuncture helps with gastrointestinal side effects. Acupuncture is predominantly tried out in neuropathy and musculoskeletal causes of pain.
There is currently a clinical trial - known as HERBAL - being conducted at National Cancer Centre of Singapore that is exploring the use of herbal medication prescribed by TCM professionals to tackle cancer-related fatigue. With that being said, we don’t generally have access to herbal treatments, so we stick to simple outpatient-based acupuncture and electroacupuncture.
CLICK HERE to read about the HERBAL trial and get enrolled to it via Oncoshot
For patients who have not recovered from neuropathy in the long term, are there any options we can further explore?
DR MOTHI: Neuropathy is a very disabling problem, though unfortunately a lot of nerve-related impairments cannot be reversed to pre-treatment levels. We always educate patients on the possibility of residual deficits but the more important thing to understand is how the deficit is affecting your function or quality of life, which can be optimised. For people who are unable to perform fine dexterity movement or certain activities because their hands are weak due to neuropathy, we do incorporate occupational therapy principals to help, along with the use of assistive devices. With mobility, however, it is not just about giving them a walking aid but how we can still make their physical activity or mobility better without assistive devices.
A lot of focus is placed on preventing falls and advising patients on how to keep their home environments safe. There are some emerging therapies, but they are still being explored in their interventional and research stages. There is something called scrambler therapy, which involves the use of a very big machine which is connected to patients’ hands and fingers to treat chronic neuropathic pain. Nonetheless, most cancer survivors experience 10 to 25 per cent of residual deficits, but the focus should be on function and quality of life, instead of reversing them.
CLICK HERE to read about a Stage 3 breast cancer survivor’s recovery journey